Honesty. Honestly?
/Thomas Jefferson said,"Honesty is the first chapter in the book of wisdom."
From childhood we’re taught to be honest. In school, we're told "Keep your eyes on your own paper."
We hear stories about famous, honest people, such as George Washington and the cherry tree (which paradoxically, may not be a true story) and Abe Lincoln, who was apparently so honest it became part of his moniker. (We probably don’t see lessons in this virtues using many modern politicians these days!)
We are instructed not to cheat at games or in sports. (Wait until you get a pro contract for that one!)
If we were raised in church, it was part of our spiritual code.
In short, we’re commanded to tell the truth. It’s drummed into our moral psyche: “Honesty is the best policy.”
But is that…well, the truth?
I mean, is honesty always the right thing to do?
Is it always a simple choice between truth and lie?
If Aunt Ethel asks “Do you like this hat?” what’s my response if I think it looks like a plastic flower arrangement exploded on her head?
If your wife asks “Do I look fat?” do you respond truthfully that you’ve noticed she’s looking plump?
And don’t get me started on Santa Claus, the Easter bunny and the Tooth Fairy!
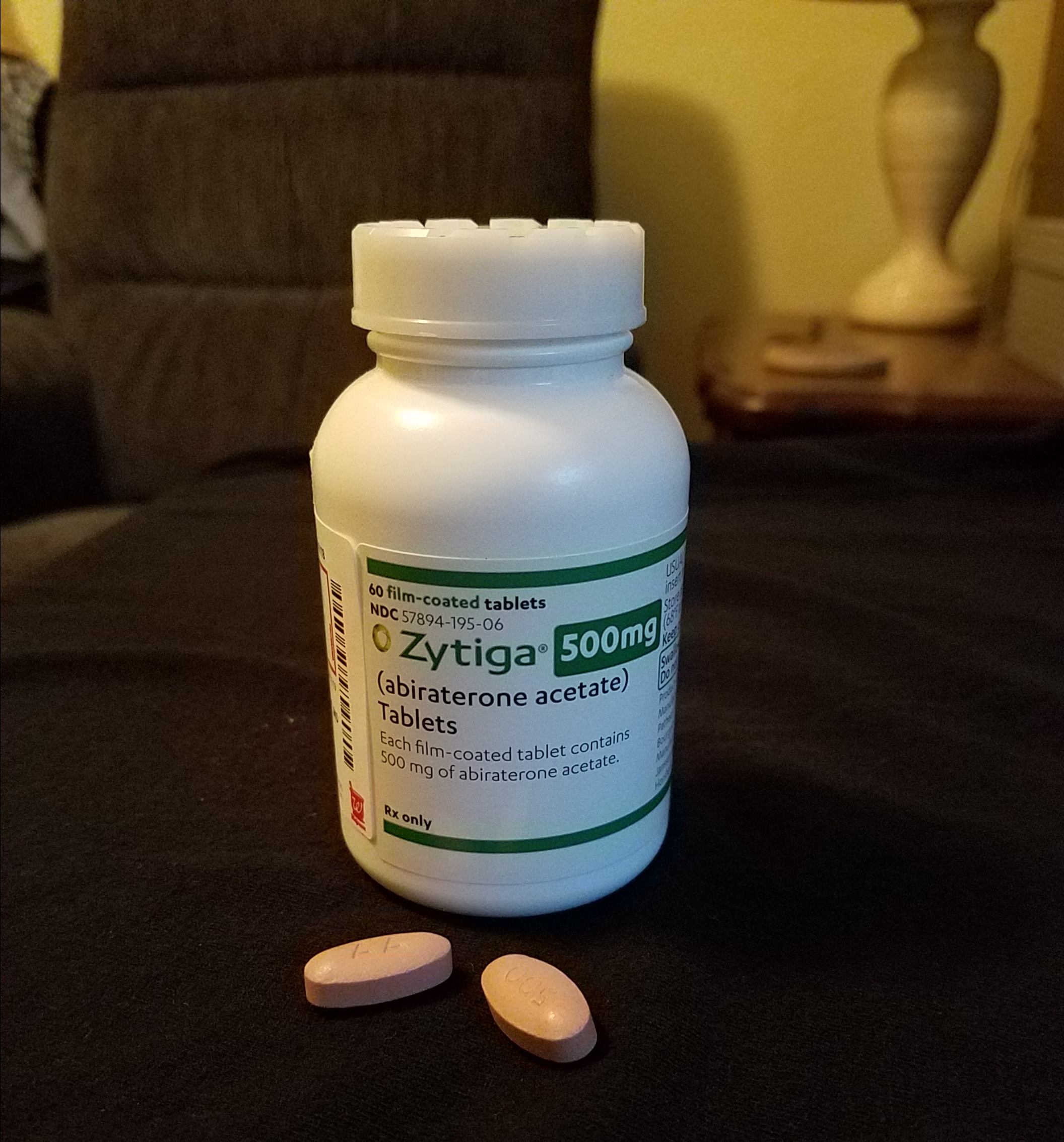
Here's my dilemma when it comes to honesty as it relates to my cancer and my treatments. I regularly get asked “How are you feeling?” It’s usually accompanied by the tilted head nod and sympathetic look. Making it worse, sometimes they'll include qualifying statements as "You look great, so how do you feel?" or "How do you feel, because you don't look sick at all?" That seems to preclude any information I should give to the contrary. (Maybe Fernando, Billy Crystal's character on SNL was right: "It's better to look good than to feel good.")
Regardless, I’m never sure how to respond because I'm not sure what they REALLY want to know. There could be genuine concern, or they're only being polite.
Am I honest, or do I lie to them?
How honest should I be?
Here’s The Truth: I rarely “feel” great; some days are better than others, but it’s all relative. I’m almost always experiencing some kind of discomfort—from achy joints to intense hot flashes to nausea to fatigue. Not to mention there are many aspects of my condition that Mom taught us should not be discussed in "polite company!" (Much of what I "feel" falls under the category of TMI—too much information.)
How do you tell someone about the frustration of out of control bodily functions that require I stay inside, and makes me afraid to be outside, not "close enough" to get to a restroom in time?
How do you explain being so tired you can barely walk, or mood swings that causes you to cry uncontrollably?
Is there a way to politely talk about how emasculating it feels to have enlarged breasts that are so sore, even a t-shirt causes pain, or being unable to be sexually intimate with my husband?
See...TMI.
I have a Pentecostal friend who tells me I should "speak" what I want as my outcome. In other words, each time someone asks how I'm doing, I'm supposed to say "I'm healed." Oh, and I should end it with "In Jesus' Name!"
Is that...honest? (There's an elaborate theology built around this concept, but it's not a faith-system I embrace! To me, it always sounded more like magical incantations.)
How are you feeling?
I don't know how to respond...honestly.
I don’t care for trite answers, such as “I'm hanging in there,” like there's a danger I might slip and fall off the planet at any second.
If I’m candid with everyone who asks, at some point, it's bound to comes across as perpetual whining or hypochondriacal complaining.
Of course, there’s always the standard courteous, perfunctory “I’m fine,” which is good decorum and probably gives them a warm and fuzzy feeling because they asked. (This is not meant to sound callous or prejudge their motives, but let’s be…truthful. Most of the time, it’s just a polite greeting, without expectations of an "organ" recital: my bladder is infected, my kidney is inflamed, my penis doesn't work, I have breasts!)
How are you feeling?
I reckon I could come up with some cleaver, witty comebacks. Of course, I'd have to avoid being rude, crude, cynical or sarcastic...and for me, that sometimes an effort. ("I feel like I might barf at any minute, so be prepared to use that hymnal as a shield!")
At times, I want to respond in my best Jack Nicholson voice: "You can't handle the truth!"
Then we have the other part of my conundrum: family and close friends who actually want to know.
And what about my husband?
In the past, I’ve resisted giving him too many details; I don’t want him to be concerned about every new symptom, side effect or pain.
I looked up the word honesty and learned it originally carried the idea of “honor” more than our modern concept of “truthful.” That helped me with a strategy. I’m working on honoring anyone who asks me, at the level of our relationship.
For the casual—those who are being polite—I will honor their civility by responding kindly, but probably without much personal investment. "I'm taking it one day at a time. Thank you for asking."
For those closest to me, I want to honor their genuine concern and be as honest as possible. "I am struggling today." "It's been a good day." And sometimes it may be: “Thanks for asking, but I don’t want to talk about it right now.”
It was William Shakespeare who told us “No legacy is so rich as honesty.”
However, the Bard also warned us to “Take note…honest is not safe.”
Honesty?
To be honest, I'm not sure!